Table of Contents
ToggleIntroduction:
The emergence and rapid spread of Candida auris, a dangerous fungal infection, have raised concerns among scientists and healthcare professionals worldwide. Recent research suggests that climate change may be a key factor behind the sudden explosion of this deadly fungus. In this article, we delve into the link between Candida auris and climate change, explore its impact on public health, and provide practical tips to mitigate its transmission. Let’s uncover the alarming truth behind this growing global threat.
Understanding Candida Auris: A Silent Menace
Candida auris is a form of yeast that typically causes no symptoms in healthy individuals. However, it poses a significant risk to patients already weakened by other medical conditions, leading to severe and invasive complications. Hospitals and nursing homes have been particularly affected by this fungal infection, making it a critical concern within healthcare settings.
Climate Change and Candida Auris: A Troubling Connection
Scientists have observed a disturbing correlation between climate change and the rise of Candida auris infections. Historically, humans and mammals have been protected from most fungal pathogens due to their warmer body temperatures. However, rising temperatures associated with climate change can enable fungi to adapt to warmer environments, potentially compromising human resistance. Candida auris’s sudden appearance in different continents suggests that it has evolved to overcome the temperature barrier that previously protected humans.
The Global Impact: Candida Auris on the Rise
Candida auris is not only a growing concern in the United States but also a global problem. In recent years, Europe has witnessed a significant increase in reported cases. Researchers attribute this rise to improved screenings, surveillance, and a genuine increase in infections. The pathogen’s resistance to traditional antifungal treatments and its alarming transmission rate have prompted public health agencies to take urgent action to mitigate its spread.
Identifying Candida Auris: Challenges in Diagnosis
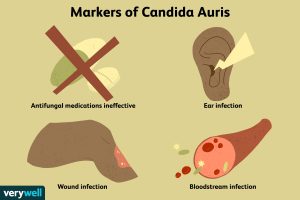
Diagnosing Candida auris can be challenging due to its rarity and lack of awareness among clinicians. Common symptoms such as sepsis, fever, and low blood pressure can have various causes, making accurate diagnosis difficult. Blood tests are often used to identify the fungus, but they may miss approximately half of the cases. Newer technologies are being developed to improve detection, but their availability in hospitals is limited.
Combating Candida Auris: Strategies for Mitigation
Efforts to combat Candida auris primarily focus on transmission mitigation in healthcare settings. Strict infection control measures, including proper hand hygiene, disinfection protocols, and patient isolation, are crucial to containing the spread of the fungus. Additionally, healthcare professionals must remain vigilant in identifying and reporting cases promptly. Collaboration between medical facilities, researchers, and public health agencies is vital in developing effective strategies and treatments.
Raising Awareness: Education and Research
Raising awareness about Candida auris is essential to ensure early detection and prompt management. Education campaigns targeting healthcare professionals, patients, and the general public can help prevent further transmission. Ongoing research is vital to better understand the fungus, its transmission patterns, and the development of more effective treatments.
Conclusion:
The sudden surge of Candida auris infections and its potential link to climate change highlights the urgent need for action. As the global healthcare community grapples with this growing threat, understanding the connection between climate change and fungal infections becomes crucial. By implementing stringent infection control measures, raising awareness, and investing in research, we can mitigate the impact of Candida auris and protect public health. Together, we can combat this alarming global challenge.
Remember, staying informed and taking proactive measures is crucial in safeguarding ourselves and future generations from the dangers posed by Candida auris and climate change.
FAQs
Q: What are Candida Auris symptoms?
A: The symptoms of Candida Auris may vary, but common signs include fever, chills, sepsis, wound infections, respiratory infections, and bloodstream infections. However, it is important to note that some individuals may exhibit no symptoms at all.



Q: What does Candida Auris cause?
A: Candida Auris can cause severe and invasive complications in individuals who are already weakened by other medical conditions. It poses a significant risk to patients in healthcare settings, leading to bloodstream infections, wound infections, and respiratory infections.
Q: What is the treatment for Candida Auris?
A: Treatment for Candida Auris infections can be challenging due to its resistance to many antifungal drugs. Healthcare professionals typically rely on a combination of antifungal medications, tailored to the specific strain and its sensitivity, to manage the infection. In some cases, removal of infected medical devices or surgical intervention may be necessary.
Q: What is the difference between Candida and Candida Auris?
A: Candida is a genus of yeast that includes various species, some of which can cause infections in humans. Candida Auris is a specific species within the Candida genus that has gained attention due to its drug resistance and ability to cause severe infections, particularly in healthcare settings.
Q: What is the main cause of Candida?
A: Candida infections are typically caused by an overgrowth of Candida yeast, most commonly Candida albicans, in the body. Factors contributing to Candida overgrowth can include weakened immune systems, prolonged use of antibiotics, hormonal imbalances, high sugar diets, and poor personal hygiene.
Q: What causes Candida in females?
A: Candida overgrowth in females, particularly in the vaginal area, can be triggered by factors such as hormonal changes (e.g., during pregnancy or menopause), the use of certain medications (e.g., antibiotics or oral contraceptives), high sugar diets, compromised immune systems, and poor genital hygiene.
Q: Can Candida cause infertility?
A: While Candida infections can cause discomfort and inflammation in the reproductive organs, there is limited evidence to suggest a direct link between Candida and infertility. However, it is advisable to seek medical attention if experiencing fertility concerns or recurrent infections.
Q: What deficiency causes Candida?
A: Nutritional deficiencies, particularly deficiencies in essential nutrients such as vitamins B6, B12, and D, magnesium, and zinc, can potentially weaken the immune system and contribute to Candida overgrowth. However, Candida overgrowth is typically multifactorial, and nutrient deficiencies alone may not be the sole cause.
Q: How to diagnose candidiasis?
A: Diagnosing candidiasis usually involves a combination of clinical evaluation, medical history assessment, physical examination, and laboratory tests. Laboratory tests may include microscopic examination of affected tissues or fluids, cultures, and molecular tests to identify the specific Candida species.
Q: Which type of fungal infection is most serious?
A: The severity of fungal infections varies depending on the specific fungus and the individual’s immune response. However, invasive fungal infections, such as those caused by Candida Auris or certain species of Aspergillus or Cryptococcus, are generally considered more serious due to their potential to spread to vital organs and cause severe complications.
Q: How is Candida auris transmitted?
A: Candida auris can spread through person-to-person contact and contaminated surfaces or equipment in healthcare settings. It can also spread indirectly through the hands of healthcare workers or contaminated medical devices. Proper infection control measures, including hand hygiene and disinfection protocols, are essential to prevent transmission.
Q: What blood test shows Candida?
A: Blood tests, such as blood cultures, can be used to detect the presence of Candida in the bloodstream. These tests help identify systemic fungal infections, including invasive Candida infections.
Q: Does Candida cause weight gain?
A: While Candida overgrowth is not directly linked to weight gain, it may contribute to imbalances in the gut microbiome and digestive system. These imbalances can affect metabolism and nutrient absorption, potentially influencing weight management in some individuals.
Q: What are the complications of candidiasis?
A: Complications of candidiasis can include the spread of the infection to other organs, the development of systemic infections, chronic or recurrent infections, and increased susceptibility to other infections. In severe cases, candidiasis can lead to sepsis, organ failure, or even death, particularly in individuals with weakened immune systems.
Q: What are normal levels of Candida?
A: Candida is a natural part of the human microbiota, and low levels of Candida are typically present in healthy individuals. However, an overgrowth or imbalance of Candida can lead to infections and related symptoms.
Q: Is Candida a serious disease?
A: Candida infections can range from mild to severe, depending on various factors such as the specific Candida species, the location of the infection, and the individual’s immune response. While mild infections are common and generally not a cause for major concern, severe or systemic infections can be serious and potentially life-threatening, especially in individuals with compromised immune systems.
Q: What is the best medicine for the treatment of candidiasis?
A: The choice of medication for treating candidiasis depends on the location and severity of the infection. Antifungal medications, such as fluconazole, itraconazole, or echinocandins, are commonly used to treat Candida infections. However, the specific medication and duration of treatment should be determined by a healthcare professional based on individual circumstances.
Q: What is Stage 4 Candida?
A: There is no recognized staging system for Candida infections. The term “Stage 4 Candida” is not a medically recognized classification and may be an inaccurate or informal reference.
Q: How long is Candida recovery?
A: The duration of Candida recovery can vary depending on the location and severity of the infection, the individual’s overall health, and the effectiveness of treatment. Mild infections may resolve within a few days to a couple of weeks, while more severe or systemic infections may require several weeks or longer for complete recovery.
Q: Is Candida permanent?
A: Candida is a normal part of the human microbiota, but an overgrowth or imbalance can lead to infections. With appropriate treatment and management, Candida infections can be resolved. However, without addressing underlying factors contributing to the overgrowth, such as weakened immune function or certain lifestyle habits, there is a risk of recurrence.
Q: How long does Candida live?
A: Candida is a naturally occurring yeast that can persist in the body. In healthy individuals, Candida is typically kept in check by the immune system and the balance of other microorganisms in the body. However, if conditions are favorable for its overgrowth, Candida can persist and cause infections until treated.
Q: What fruits can I eat on Candida diet?
A: The Candida diet typically restricts high-sugar fruits due to their potential to promote Candida overgrowth. Low-sugar fruits, such as berries (e.g., blueberries, raspberries, strawberries), green apples, and lemons, are often considered more suitable for a Candida diet. However, individual dietary preferences and tolerances may vary, so it is advisable to consult with a healthcare professional or nutritionist for personalized dietary guidance.
Q: What happens when Candida dies?
A: When Candida cells die, they are typically broken down and eliminated by the body’s immune system and natural processes. However, the release of cellular components during Candida cell death can trigger an inflammatory response in some individuals, leading to a temporary worsening of symptoms before improvement occurs.
Q: Is candidiasis curable?
A: Candidiasis is generally treatable with appropriate medical intervention, including antifungal medications and addressing underlying factors contributing to the overgrowth. However, it is important to note that recurrence is possible, especially if predisposing factors are not addressed.
Q: What are natural antifungal foods?
A: Some natural foods possess antifungal properties and may help in managing Candida overgrowth. Examples include garlic, coconut oil, oregano oil, apple cider vinegar, ginger, and pau d’arco tea. However, the effectiveness of these natural remedies may vary, and it is advisable to consult with a healthcare professional before relying solely on them for treatment.
Q: Can Candida be removed?
A: Candida is a part of the normal microbiota, and complete eradication is not typically necessary or possible. However, Candida overgrowth and associated infections can be effectively managed and controlled through appropriate medical treatment, lifestyle modifications, and dietary changes.
Q: Symptoms of Candida auris in adults?
A: Symptoms of Candida auris in adults can include fever, chills, wound infections, respiratory infections, bloodstream infections, and sepsis. However, it is important to note that some individuals may exhibit no symptoms or only mild symptoms.
Q: Where is Candida auris found?
A: Candida auris has been found in various countries across the globe, including the United States, Europe, Asia, and South America. It can primarily be found in healthcare settings, such as hospitals and nursing homes, where transmission can occur between patients and on contaminated surfaces or medical equipment.
Q: What kills Candida auris naturally?
A: Candida auris is highly resistant to many antifungal medications, making it difficult to treat. Natural remedies alone are unlikely to effectively eliminate Candida auris. Medical intervention, including appropriate antifungal medications, infection control measures, and strict adherence to infection prevention protocols, is necessary to combat Candida auris infections