Table of Contents
ToggleIntroduction
Antimicrobial resistance (AMR) is a critical global health issue that has been evolving over the past few decades. From 1990 to 2021, the impact of AMR on human health has been profound, with significant variations in burden across different regions and age groups. This article delves into a detailed analysis of AMR trends, providing insights into past data and future projections. Let’s explore how AMR has affected global health and what the future might hold if current trends continue.
Understanding Antimicrobial Resistance
What is AMR?
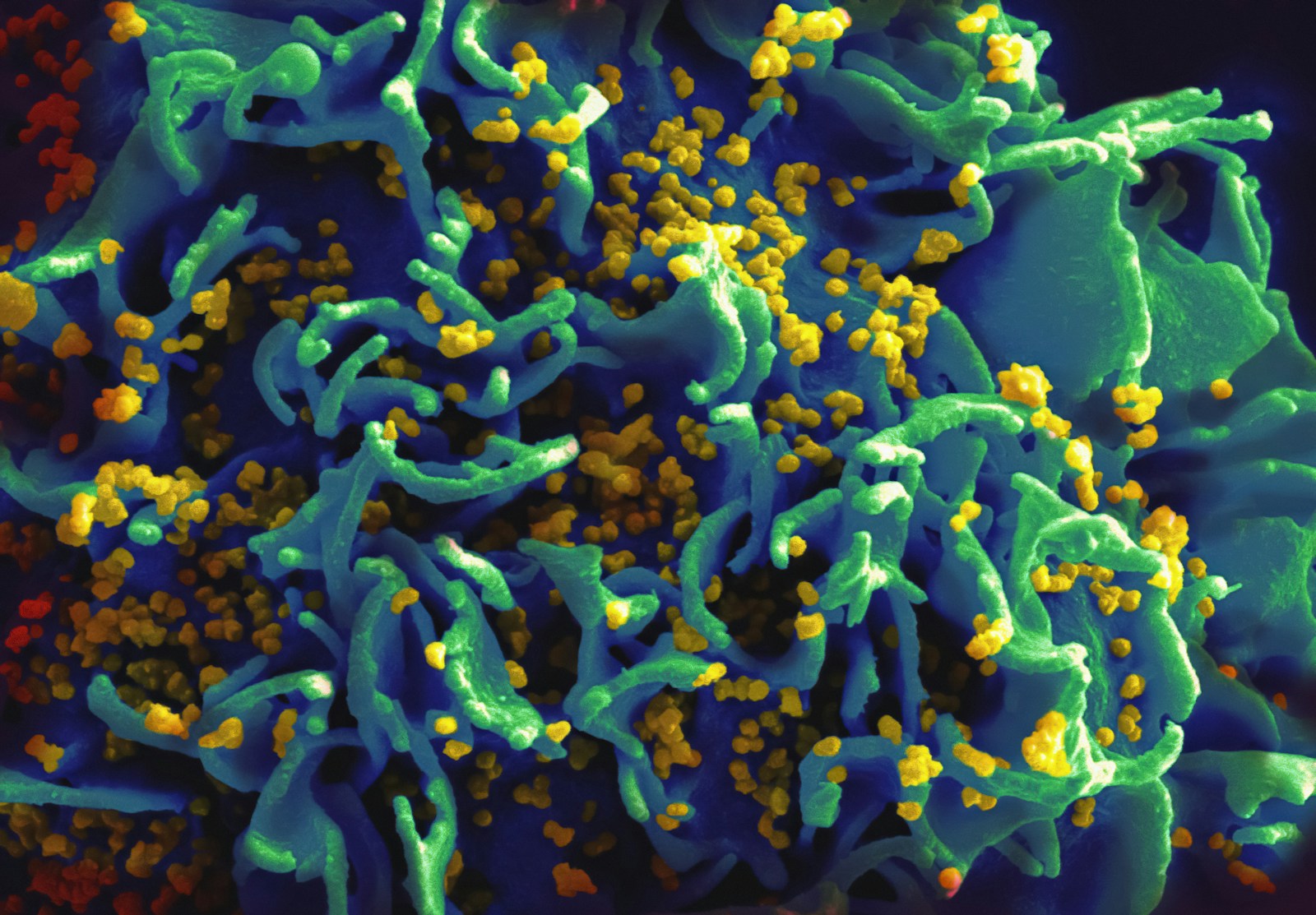
Antimicrobial resistance occurs when bacteria evolve to resist the effects of drugs that once killed them or inhibited their growth. This makes infections harder to treat and increases the risk of severe illness and death. AMR is driven by various factors, including overuse and misuse of antibiotics in medicine and agriculture.
Historical Trends in AMR (1990–2021)
Global Overview
From 1990 to 2021, the global burden of AMR has fluctuated significantly. Initially, AMR was a growing concern, but recent data reveal a more nuanced picture. The total number of deaths associated with bacterial AMR in 2021 was estimated at 4.71 million, with 1.14 million deaths directly attributable to AMR.
Regional Variations
AMR’s impact has varied widely by region. For instance, while deaths from AMR decreased by over 50% among children under 5 years globally, the situation worsened for older adults. Deaths among individuals aged 70 and above increased by over 80% in the same period.
Key Findings from 1990 to 2021
Rise in Resistant Pathogens
One of the most notable trends is the increase in deaths associated with meticillin-resistant Staphylococcus aureus (MRSA). Globally, MRSA-related deaths rose from 261,000 in 1990 to 550,000 in 2021. Similarly, resistance to carbapenems, a class of antibiotics used to treat severe infections, also increased significantly.
Decrease in Non-COVID-Related Infectious Diseases
In 2020 and 2021, there was a notable decrease in non-COVID-related infectious diseases, which might reflect changes in healthcare priorities and pandemic-related shifts in health service delivery.
Forecasting AMR Impact to 2050
Projected Deaths and DALYs
Looking ahead to 2050, projections indicate a significant rise in AMR-related deaths. The forecast suggests that 1.91 million deaths directly attributable to AMR could occur, with 8.22 million deaths associated with AMR. The most affected regions are likely to be South Asia and Latin America.
Age-Related Trends
The increase in AMR-related deaths is expected to be most pronounced among the elderly. By 2050, individuals aged 70 and above will account for nearly 66% of all AMR-related deaths. This trend highlights the growing need for targeted interventions for older populations.
Future Scenarios
Better Care Scenario
Under a scenario where healthcare quality improves, and access to appropriate antibiotics increases, up to 92 million deaths could be averted between 2025 and 2050. This underscores the potential benefits of enhanced healthcare systems and improved infection management.
Gram-Negative Drug Scenario
If new drugs targeting Gram-negative bacteria are developed, approximately 11.1 million AMR deaths could be prevented. This scenario emphasizes the importance of ongoing research and development in combating AMR.
Strategies for Mitigating AMR
Infection Prevention and Control
Preventing infections through vaccination and improved hygiene practices is crucial. The reduction in AMR deaths among younger children illustrates the effectiveness of preventive measures.
Antibiotic Stewardship
Minimizing the misuse of antibiotics in both humans and animals is essential to slow the spread of resistance. Efforts should focus on reducing unnecessary prescriptions and promoting appropriate use.
Research and Development
Investing in new antibiotics and alternative treatments is vital. Continued research can help address gaps in current treatment options and develop new strategies to combat resistant pathogens.
Policy and Education
Governments and organizations should implement policies that promote responsible antibiotic use and support educational initiatives to raise awareness about AMR.
Conclusion
The global burden of bacterial antimicrobial resistance presents a significant challenge for public health. While progress has been made in some areas, the rising trends of AMR-related deaths, particularly among older adults, underscore the need for continued vigilance and action. By focusing on prevention, responsible antibiotic use, and research, we can work towards mitigating the future impact of AMR and safeguarding global health.
FAQs
1. What is antimicrobial resistance (AMR)?
Antimicrobial resistance occurs when bacteria develop resistance to antibiotics that were once effective in treating infections. This makes infections harder to treat and increases the risk of severe outcomes.
2. How has AMR affected different age groups?
AMR-related deaths have decreased among children under 5 years but have increased significantly among older adults, particularly those aged 70 and above.
3. What are the main contributors to AMR?
The primary contributors to AMR include the overuse and misuse of antibiotics in both medicine and agriculture, as well as poor infection prevention practices.
4. What can be done to prevent AMR?
Prevention strategies include improving infection control practices, reducing unnecessary antibiotic use, investing in new drug development, and promoting public awareness.
5. How can new drugs help in combating AMR?
Developing new drugs, especially those targeting Gram-negative bacteria, can help address the growing resistance and provide effective treatment options for resistant infections.